Welcome
|
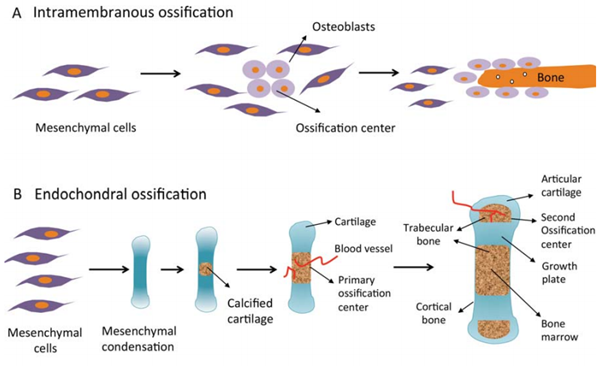
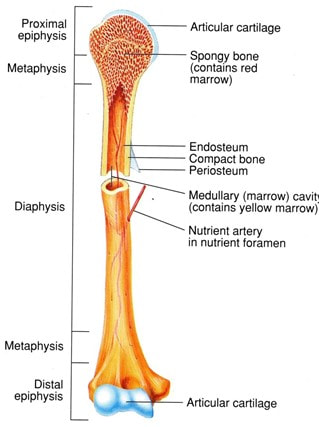
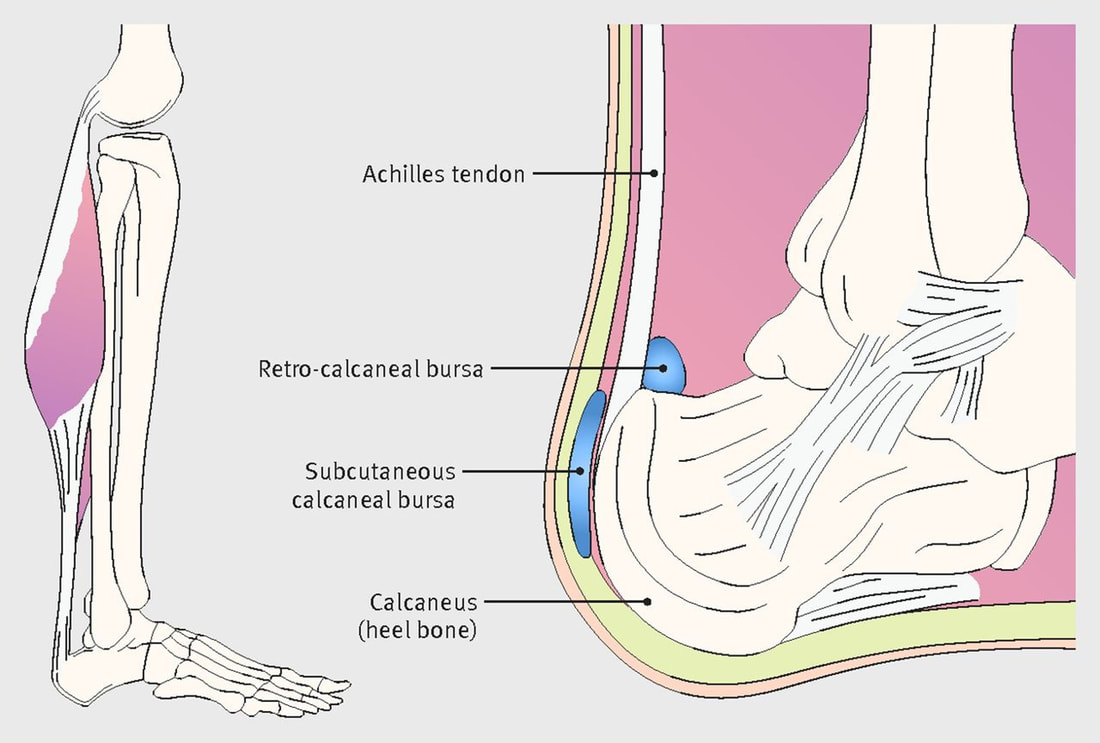
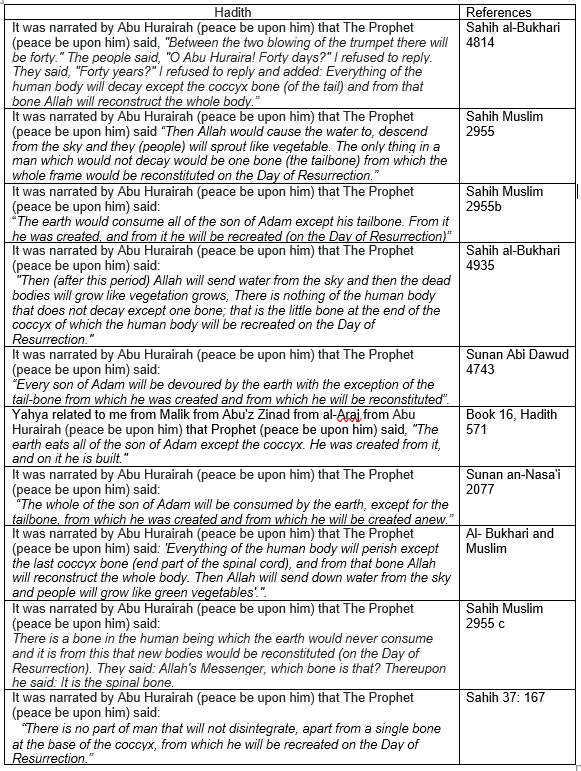
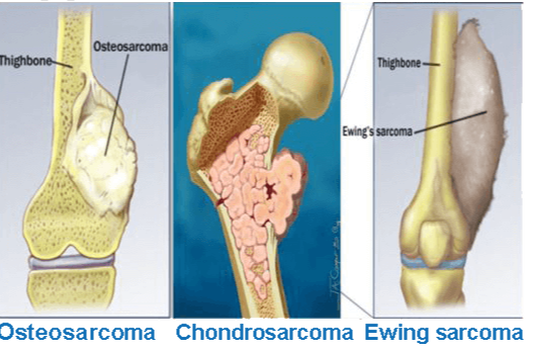
The anatomical and physiological context of the heart and how the red blood cells (erythrocytes) carry oxygen around the body via the blood was discussed last month. This was achieved using core evidence from the Quran, Hadith, and literature work by scholars in the fields of Islam and medicine. Today, this section of the project aims to continue bridging the gross anatomy and physiology of the human body with the foundations of Islam by discussing the structure and function of the bone; this is where red blood cells are made via the process known as erythropoiesis. Besides, we will also cover other elements of the musculoskeletal system, the joints, muscles, cartilages, tendons and the ligaments. In total, the bone has been stated in the Quran twelve times. Allah (The Most High) states: “Or are you not aware of˺ the one who passed by a city which was in ruins. He wondered, “How could Allah bring this back to life after its destruction?” So Allah caused him to die for a hundred years then brought him back to life. Allah asked, “How long have you remained ˹in this state˺?” He replied, “Perhaps a day or part of a day.” Allah said, “No! You have remained here for a hundred years! Just look at your food and drink—they have not spoiled. ˹But now˺ look at ˹the remains of˺ your donkey! And ˹so˺ We have made you into a sign for humanity. And look at the bones ˹of the donkey˺, how We bring them together then clothe them with flesh!”1 When this was made clear to him, he declared, “˹Now˺ I know that Allah is Most Capable of everything.” [Quran, Surah Baqarah (The Cow), 2:259] A number of respected scholars: Ibn Jarir, Ibn Abi Hatim, Ibn Abbad, Al-Hassan, Qatadah, Al-Suddi and Sulaiman bin Buradysh (may Allah have mercy upon them all) agreed that this Quranic verse is a reference to the story of Uzayr that took place in Jerusalem after Nebuchadnezzar destroyed it and killed its people (Abi Hatim, 3:1009; Al-Tabari 5:439; Al-Tabari 5:440; Ibn Kathir, 2000). He was resurrected by Allah (The Most High) and asked whether he was 'dead a day or part of the day'. Al-Hakim (may Allah have mercy upon him) in his book Mustadrak mentioned that Kharijah bin Zaid bin Thabit (may Allah have mercy upon him) mentioned that his father said that the Prophet (peace be upon him) used the term 'Nunshizuha' is in relation to adjustment. However, this was not recorded Sahih by Bukhari and Muslim (2:234). It was mentioned by Mujahid it was 'nunseeha' (Al Tabari 5:476). Al-Suddi (may Allah have mercy upon him) further added that Uzayr witnessed the bones of his donkey being collected and Allah (The Most High) covered the bones with flesh, nerves, veins and skin and brought life into the donkey via the nostrils (Ibn Kathir, 2000). This consolidated Uzayr's faith in the Almighty that He can do All things and is Most Knowledgeable (Ibn Kathir, 2000). It also presents Allah’s instructions to research closer into the gross anatomy of the bone on how ‘we construct them’ for clarity and belief. The functions of the musculoskeletal system are the movement with levers of muscles, support, and posture. For Muslims, particularly the bone is essential to perform our daily prayers (Salah) and the coccyx is the form in how humanity will be resurrected in the afterlife. In Figure 1, it illustrates the positions in which human prostate to the Almighty. This corresponds to the hadith narrated by Ibn Abbas (may Allah have mercy upon him): "The Prophet peace be upon him was ordered by Allah (The Most High) to prostrate on seven parts and not to tuck up the clothes or hair whilst praying. Those parts are the forehead along with the tip of the nose, both hands, both knees and the toes of both feet." [Al-Bukhari, 809] Ahmad (2010) shared evidence that praying increases the strength of bones and improves the spinal curvature. The strength of the muscles depends on pressure and muscle contraction. Inactivity causes the electric current in the bones between the two poles to decrease and weaken the bones. Similarly, this can also occur in space where the movement is weakened because there is no resistant force of gravity. This emphasises how atrophy can influence movement and bone metabolism. The daily prayer involves 17 units/rakaahs and this excludes the voluntary prayers. It is estimated it takes ca. two hours, on the other hand, it is important to state that there is no exact time to complete the prayer because it depends on the pace, Surah read and other factors (Ahmad, 2010). The divine energy that flows through the heart and body motivates to continue to the straight path. Figure 1: The bone positions for prostration. Furthermore, there is also evidence of movement in the Quran, where Allah (The Most High) states: "And Allah has created from water every living creature. Some of them crawl on their bellies, some walk on two legs, and some walk on four. Allah creates whatever He wills. Surely Allah is Most Capable of everything." [The Quran, Surah Al-Noor (The Light), 24:45] Ibn Kathir (2000) mentioned that Allah created living things in different forms and colours. The snakes crawl on their bellies whilst humans and bird walk on two legs. Cattle, horses, lions, and camels are examples of living creatures that walk on 4 legs. The description of how living creatures can move ignites guidance, understanding and intellect for people to ponder. Nevertheless, there are also differences whereby despite; humans and birds both walk on two legs, they differ in the torso position and posture. Furthermore, Allah states in the following verse how man is a witness against himself. "Rather, man, against himself, will be a witness." [Quran, Surah Al-Qiyamah (The Resurrection), 75:14] Qatadah (may Allah have mercy upon him) mentioned in a narration 'By Allah! If you wish to see him, you would see him as someone who sees the shortcomings of the people and their sins, yet he is heedless of his own sins. It used to be said, "Verily, it is written in the Injil; `O Son of Adam, do you see the small splinters in the eye of your brother and disregard the tree stump that is in your eye, so you do not see it." (Al Tabari: 24:62; Ibn Kathir, 2000). Other functions of the musculoskeletal system are the formation of blood cells (haematopoiesis), maintenance of the homeostasis for calcium and phosphate mineral ions that aids in the production of cytokines and growth factors and the protection of vital organs such as the brain, heart, and the lungs because of the strength and rigidity of the bone (Clarke, 2008; Ralston, 2017). the development of the boneThe human skeleton accounts for 20% of the body weight. The number of bones of the human skeleton at birth is 98, which later develops into 270 bones (Scheuer and Black, 2000). The adult skeleton has 206 bones and this is because of the remodelling of the bones where the fusion between the bones takes place. This decreases the number of bones preserving their strength and rigidity. For instance, a child has five sections of the sacral vertebrae and develops into one section when transitioning into an adult (Scheuer and Black, 2000). The human skeleton is presented in Figure 2. There are two types of the human skeleton: axial and appendicular skeleton. The axial skeleton consists of the cranium (head), vertebrae and the neck (cervical and hyoid vertebrae)(Clarke, 2008). The appendicular skeleton consists of the upper and lower limbs, for instance, the pelvic girdle and the shoulders. In some literature, there is an additional type - the visceral skeleton that consists of the sternum, ribs, lower and upper jaw (Al-Najjar, 2005). However, other sources suggest that there are 213 bones, and this excludes the sesamoid bones: the appendicular skeleton has 126 bones, the axial skeleton has 74 bones and; there are 6 bones in the auditory ossicles (Clarke, 2008). Bones vary in size, structure, and markings and this makes it adaptable to its location and function in the human body. There are three types of bone markings: articulation, holes, and projections. Articulation is where bones are joined together that specifically fit. Holes are opening grooves in the bone that allow blood vessels and nerves to enter. The projection is found on the bone surface that serves a place where tendons join muscle to bone and ligaments bone to bone (OpenStaxCollege, n.d.). The bone consists of 25% of organic products (glycoproteins, proteoglycans, and collagens) and 75% of calcium salts. Figure 2: The human skeleton 6During the fetal development which occurs between the 3rd and 8th week, Allah (The Most High) created the vertebrae (backbone) from cartilage before the muscles. The jawbone (mandible) is the first cartilage (Meckel's cartilage) that underwent transition into a bone on Day 41. The cartilage is a semi-rigid connective tissue that acts as a shock absorber. It provides support and adds a smooth surface for the articulation of the bones to grow and develop and perform gliding movements (Yusof et al., 2016). Three types of cartilage differ in the number of extracellular fibres: the hyaline cartilage has several fibres but do not have perichondrium and cannot regenerate new cartilage following injury, the fibrocartilage comprises of collagen fibres and the elastic cartilages contains elastic fibres (Young et al., 2006). Allah (The Most High) states: "Verily, We have created the human from a quintessence of clay; then We placed him as a drop in a fixed resting place. We then made the drop into a clot and that into a fetus. We then made bones and clothed the bones with flesh and from that brought forth another creation. Therefore, blessed is God, the very best of those who create." [Quran, Surah Al-Muminoon (The Believers, 23:12-14]Ibn Kathir (2000) mentioned concerning the bones that they were clothed with flesh to cover and strengthen the body. There are nerves and veins in the head, two arms and two legs. This highlights the uniqueness and vivid detail of the physical creation of man portrayed by Allah (The Most High). It also contemplates the findings of Wyganowska-Swiatkowska and Przystanska (2011) who discovered that at 32 days, the Meckel's cartilage developed and ossification is progressed at 41 days where a mandible is formed inferior to the cartilage where the muscles begin to form at 44 days. The formation of the bone is known as osteogenesis or ossification. It occurs from the neural crest, paraxial mesoderm or lateral plate that become somites and differentiate into sclerotome and dermatomyotome cells (Moore and Persaud, 1998). Further differentiation occurs where the sclerotome cells produce the connective mesenchyme that later forms the bone-forming cells called osteoblasts, fibroblasts and chondroblasts. There are two ways in how the bones are formed: intramembranous and endochondral ossification illustrated in Figure 3. Intramembranous ossification is where the mesenchymal cells transition into osteoblasts without the formation of cartilage. There is a high vasculature area of the embryonic connective tissue (primary ossification) and; the bones can be re-shaped to form lamellar bone. The limb buds later form the upper and lower limbs and comprise of; the apical ectodermal ridge (AER) and cuboidal ectoderm. Endochondral ossification is where the bone is produced via cartilage, the chondrocytes proliferate and undergo maturation to form bone (Tzelepi et al. 2009). The canonical Wnt/β-catenin pathway is fundamental in the differentiation of the osteoblasts, chondrogenesis and haemopoiesis (Clarke, 2008). The Wnt (wingless) proteins produce the dermatomyotome that expresses the muscle-specific genes e.g. MYF5 to stimulate the synthesis of skeletal muscles (Sadler and Langman, 2010). Figure 3: Ossification (Creative Biomart, 2020) the gross anatomy of the bone.The bone (osseous) tissue consists of connective tissue (collagen type I fibres) that aids in its elasticity and the mineral salts (inorganic salts) that provide its hardness and rigidity. Calcium phosphate and carbonate produce hydroxyapatite and adheres to the collagen fibres. There are additional mineral ions, for instance, fluoride, magnesium hydroxide and sulphate that calcify the collagen fibres to increase the flexibility (Clarke, 2008). The histological macrostructure of the bone is dependent on its porosity: cortical (compact) bone and trabecular bone (cancellous/spongy) bone (OpenStaxCollege, n.d.) presented in Figure 4. The human skeleton has 80% compact bone and 20% cancellous bone (Eriksen et al. 1994). There is variation in the ratio of compact and cancellous bone in the human skeleton, for instance, the femoral head has 50:50 ratio between compact to cancellous bones, respectively. On the other hand, the vertebrae have more cancellous tissue where the ratio proportion is 25:75 in respect to the ratio: compact to cancellous bones (Clarke, 2008). This highlights how the structure and the remodelling of the bone make it adaptable to its function. The microstructural unit of the bone is osteons (Haversian systems). They are 400 mm long and 200 mm wide in the compact bone (Clarke, 2008). The osteons produce concentric rings (lamellae) in the compact bone. The cancellous bone has semilunar osteons ca. 35 m thick in the lacunae producing a lattice-like matrix called trabeculae (Yusof et al., 2016). The compact bone is found in the shafts of long bones in particularly the periosteum and diaphysis. It is less metabolically active than the cancellous bone and functions in providing mechanical strength and protection from internal and external forces (Clarke, 2008). The biomechanical forces can be felt at the osteocyte syncytium of the bone via the canalicular network and the gap junctions (Clarke, 2008). Cancellous bone has rods and plates and consists of marrow cavities to bear the load. There is red marrow between the cells to provide balance and; withhold the density of the compact bone and; this lightens the weight of the bone and allow the muscles to function. Figure 4: The anatomy of the bone TYPES OF BONESThere are four main types of bones: short, flat, long, and irregular bones. Long bones are produced by intermembranous and endochondral formation. It is found in the clavicle, humerus, ulnae, femur, radius, phalanges, and metatarsals. Short bones are found in the patella, sesamoid, carpal, and tarsal bones. Irregular bones are found in the vertebrae, coccyx, hyoid, and sacrum. Flat bones are found in the mandible, skull, sternum, ribs and scapulas and formed by membranous ossification (OpenStaxCollege, n.d.). This illustrates the unique creation of Allah (The Most High) in how he created each bone with its adaptable functions. Amongst the verses in the Quran that emphasize Allah's Divine ability to create is: “Allah is the Creator of all things, and He is the Wakil (Trustee, Disposer of all affairs, Guardian) over all things.” To him belong the maqalid of the heavens and the earth. And those who disbelieve in the Ayat of Allah such are they who will be losers. [Quran, Surah Al Zumr (The Groups, 39:62 63] This suggests that Allah (The Most High) encourages mankind to research nature and its molecular, cellular and biochemical composition to understand how they function. The Merciful even provided clues to His creation for guidance to The Truth. For Allah (The Most High) has the power to create, command and whatever He decides is fair and just (Ibn Kathir, 2000). The long bone consists of two parts: diaphysis and epiphysis. The diaphysis is a tubular shaft that initials in the proximal end of the bone and continues to the distal end. The epiphysis is the wider area of the bone. The epiphysis connects with the diaphysis at the metaphysis. The metaphysis is a narrow area that is composed of a transparent hyaline layer of cartilage and the epiphyseal plate otherwise known as the growth plate as presented in Figure 5. It then progressed to adult bones where the cartilage and epiphyseal plate transitions to osseous tissue and epiphyseal line respectively (OpenStaxCollege, n.d.). The walls of the diaphysis of the long bone are made of compact bone that is dense and hard. The yellow marrow is present in the hollow region of the diaphysis called the medullary cavity as presented in Figure 5a. There are two membranes periosteum and endosteum. There is a thin membrane that surrounds the medullary cavity called the endosteum. The red marrow fills the spongy bone of the epiphysis. There is another outer membrane that is fibrous called the periosteum that covers all the bone with exception of the connection where epiphyses form joints with other bones where there is a thin layer of articular cartilage instead of the periosteum to decrease friction. The periosteum is surrounded by thick collagen fibres called Sharpey”s fibres extending under the bone tissue. The periosteum comprises of blood and lymphatic vessels and nerves that provide a nutrient supply for the compact bones. The compact bone nourishes the spongy bone and medullary cavity that coils around the venous marrow longitudinal vein (OpenStaxCollege, n.d.). Arteries connect with diaphysis and enter through small openings called foramen. The arteries divide into ascending and descending branches that are parallel into thin-walled arterioles and capillaries (Travlos, 2006). The veins also pass-through marrow cavities and exit via foramena. The venous sinuses are thin-walled and have endothelial cells with minor basement membrane (Travlos, 2006). There are myelinated and non-myelinated nerves that have the smooth muscle of the arterioles (Travlos, 2006). The cranium has a spongy bone on each side of rhe compact bone called a dipole to protect the internal organs from fracture and injury (OpenStaxCollege, n.d.) Think about it, if Allah (The Most High) added detail to a snowflake - Figure 5b that is left for mankind to ponder and eventually melts. Contemplate on the beautiful creation of the bone presented in Figure 5a. “Which is it, of the Favours of your Lord, that ye deny?” [Quran, Surah Al-Rahman (The Most Merciful), 55:13] Figure 5. The creation of the bone and snowflake (a) The structure of the long bone (b) snowflake (Imster, 2019) the cellular features of the boneThere are four types of bone cells present in the osseous tissue: osteogenic cells, osteoblasts, osteocytes, and osteoclasts. The undifferentiated osteogenic cells arise from pluripotent stem cells under optimal conditions. It resides in the periosteum and bone marrow and has a high mitotic activity to produce osteoblasts and maintain its levels to produce new bone matrix (Clarke, 2008). The osteoprogenitor lineage regulates the expression of bone morphogenetic proteins (BMP) and Wingless (Wnt) proteins to induce differentiation of osteoblasts (Canalis et al. 2003). Osteoblasts are cuboidal cells that reside in the periosteum and endosteum and accounts to 4 to 6 % of all bone cells. They have a high amount of rough endoplasmic reticulum (RER), Golgi apparatus and secretory vesicles to produce proteins (collage) and secrete osteoid tissue in the matrix. The function of the osteoblasts is to produce new bone and; this involves several transcription factors Runt-related transcription factor 2 (RUNX2) gene, Osterix (Osx) and Distal-less homeobox that upregulates bone matrix proteins: osteocalcin (OCN), alkaline phosphatase (ALP) and bone sialoprotein (BSP) (Fukumoto and Martin, 2009; Marks and Popoff, 1988). It later becomes trapped in the calcified bone matrix where their structure and function alter from mature osteoblasts to form osteocytes; the most common form of bone cells (Ducy et al., 1997). This alters the ultrastructure of the cells and their size. The RER and Golgi apparatus decreases and the protein synthesis and secretion decreases (Schaffler et al. 2014). Osteocytes are situated in the lacunae in adjacent lamellae that form matrix channels (canaliculi) to create the central canal. The central canal consists of nerves and blood vessels that form a branched network called Volkmann's canals (perforating canal) and; this extends from the two membranes periosteum and endosteum and therefore; acts as a nutrient supply and removes waste products. This, in turn, supports the structure of the bone and the surface of the Quiescent bone lining cells (BLCs) (Clarke, 2008). It is important to state that the canaliculi are essential for the communication of osteoblasts and osteocytes because they do not undergo mitosis as opposed to the osteogenic stem cells that have mitotic activity. Osteocytes are metabolically active and secrete various enzymes and matrix proteins for adhesion and to maintain the mineral concentration in the calcified bone matrix. They also express OCN and a cell adhesion receptor called CD44 to produce a bone matrix protein called hyaluronate and this is essential for the structure and metabolism of the bone (OpenStaxCollege, n.d.). Furthermore, osteocytes secrete integral cellular proteins, for example, connexins maintain the gap junctions between bone cells. Gap junctions are required for maturation, activity, and survival of osteocytes (Clarke, 2008). Besides, osteocytes secrete lysosomes and can act as phagocytes (Clarke, 2008). BONE HOMEOSTASISBones are formed by the osteoblasts whereas; the osteoclasts dissolve the old proteinaceous matrix. This releases the calcium ions, repair, and remodels to form new osseous tissue. The osteocytes act as a mechanosensory stimulator for the bone-remodelling process and participate in the osteoblastic and osteoclastic activities (Florencio-Silva et al. 2015). Bone homeostasis is regulated by local and systemic factors: systemic factors include parathyroid hormones, calcitonin and oestrogen hormone whereas local factors include cytokines and growth factors (Florencio-Silva et al. 2015). Osteoclasts and osteoblasts are multinucleated bone cells that develop from mononuclear precursor cells of the monocyte-macrophage lineage (Clarke, 2008; OpenStaxCollege, n.d.). This is facilitated by two cytokines produced by marrow stromal cells: receptor activator of NF-κB ligand (RANKL) and the macrophage/monocyte colony-stimulating factor (M-CSF). RANKL belongs to the Tumour Necrosis factor (TNF) family are needed for the differentiation, proliferation, and survival of cells. M-CSF binds to its receptor c-Fms to stimulate the recruitment of adaptor proteins and cytosolic kinases to induce cellular signalling. There is crosstalk between M-CSF and RANKL, where M-CSF can stimulate the RANKL-RANK-OPG signalling pathway that regulates the production and maturation of the osteoclasts (Al-Bari and Al Mamun, 2020). OPG is a membrane-bound protein that prevents the association of RANKL with its receptor (Clarke, 2008; Al-Bari and Al Mamun, 2020). Overexpression of OPG causes osteopetrosis where there is a deficiency of the osteoclasts, however, when the deletion of OPG occurs, it causes overactivity of the osteoclasts leading to osteoporosis. Dysregulation of the remodelling process influences the calcium and phosphate homeostasis causing fracture, pain and deformity (Ralston, 2017; Yin et al., 2019). Another factor that stimulates osteoclastogenesis is tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) receptors that activate TRAF6 and receptor activator of nuclear factor‐κB (NF‐κB) signalling pathways which upregulates the expression of nuclear factor of activated T cells cytoplasmic 1 (NFATc1) (Clark, 2008). Resorption of the bone is facilitated by hydrogen ions, metalloproteinases, cathepsin K enzyme and microtubules. Hydrogen ions are produced by the chloride channels and the enzyme H+ ATPases and; it acidifies the area of resorption that contains type I collagen. The B1 family of integrin receptors in the membranes of the osteoclasts binds to the peptides present in the bone matrix via the actin filament. This forms a sealed actin ring and; the matrix become polarised. Examples of peptides are laminin, fibronectin, osteopontin and sialoprotein. Resorption of the bone can be evaded if the actin ring is blocked. The resorbing osteoclasts transition into actin-containing podosomes that attach to the matrix (Clarke, 2008). Recent studies suggest that autophagic activity can affect bone homeostasis that can cause osteoporosis (Yin et al., 2019). Osteoblasts, osteoclasts and osteocytes have a basal level of autophagic activity where it contributes to their differentiation, functioning and survival in hypertonic, hypoxic and nutrition-deficient environments (Nollet et al. 2014; Zhu et al. 2017; Zheng et al. 2017; Dallas et al. 2013; Shapiro et al. 2014) BONE MARROWThe bone marrow is a soft, gelatinous, lymphoid tissue found in the medullary cavities of trabecular bone and there are two types: red bone marrow consists of haematopoietic/myeloid tissue and yellow bone marrow consists of adipose tissue surrounded by vascular sinuses and capillaries (Travlos, 2006; Allied academies, 2020). It is considered one of the largest organs in the body and accounts ~ 5% of the body weight. It is particularly found in the hip and thigh bones. A multidisciplinary approach can be performed to understand and evaluate the composition of the bone marrow through peripheral blood examination in toxicity studies, bone smears, iron stores, bone marrow aspirates and tissue sections through histological examination to determine alterations and architecture of the cells and tissues for inflammation and other pathological features (Travlos, 2006). The bone marrow has been mentioned in one of the hadiths narrated by Abu Hurairah (may Allah have mercy upon him) that Prophet (peace be upon him) said: “The first batch (of people) who will enter Paradise will be (glittering) like the full moon, and the batch next to them will be (glittering) like the most brilliant star in the sky. Their hearts will be as if the heart of a single man, for they will have neither enmity nor jealousy amongst themselves; everyone will have two wives from the houris, (who will be so beautiful, pure and transparent that) the marrow of the bones of their legs will be seen through the bones and the flesh." [Hadith, Al Bukhari, 3254] There are also haematopoietic and mesenchymal stem cells found in the bone marrow producing red blood cells (erythropoiesis), white blood cells (lymphopoiesis; granulopoiesis) and platelets (megakaryocytopoiesis). This maintains the self-renewal process of pluripotent stem cells and results in the differentiation and maturation of cells – the colony-forming unit is granulocytes, erythrocytes, monocytes, and megakaryocytes (CFU-GEMM) (Travlos, 2006) Many people with anaemia and blood cancers (leukaemia and lymphoma) rely on bone marrow or cord blood transplants to survive. When a disease outbreaks and affects the bone marrow, it causes the bone marrow not to function effectively. This is treated with marrow or cord blood transplant. Erythrocytes illustrated in Figure 6 are produced in the erythroblastic islands and are regulated by the humoral factor, erythropoietin that is primarily produced in the kidneys and small aliquots are found in the liver. Erythropoietin proliferates the progenitor cells and increases the differentiation and maturation of erythrocytes (Travlos, 2006). Erythropoiesis is also regulated by hormones of the gonads, adrenal, pituitary and thyroid glands. Growth hormone, androgens and thyroxine stimulate the production of erythropoietin. Oestrogen has an inhibitory effect that maintains the levels of erythropoietin (Karsten et al. 2018). The pro-inflammatory factors that are involved in erythrocytes are interferons (IFN-α2; IFN-γ); interleukins (IL-1α, -5, -9, -12, -15, -17 and -18), TRAIL, TNF and Macrophage migration inhibitory factor (MIF) (Karsten et al., 2018). The anti-inflammatory factors that are involved in erythrocytes are the following cytokines: IL-4,-10 and -13. Figure 6: Erythrocytes Lymphopoiesis takes place in the bone marrow microenvironment whereas; T cell lymphopoiesis takes place in the thymus. There are heavy chains present in the pre-B cells that vary by size. The size of the smaller pre-B cells are ca. 9 microns and mature into B cells. The larger pre-B cells express A and K chains and are regulated by the stromal cells. Other cells are produced in other locations, for instance, granulocytes are synthesised in distinctive focis and platelets are produced adjacent to the endothelium (Travlos, 2006). Other cytokines are also involved in the regulation of cellular differentiation and maturation in the haematopoietic microenvironment. IL-2 and IL-3 produce macrophage and myeloid cells respectively. IL-3 also produces T lymphocytes. Burst promoting activity (BPA) is produced by T-lymphocytes and macrophages. Bone morphogenetic protein 6 (BMP-6) regulates chondrogenesis, osteogenesis and decreases osteoclastic differentiation via IL-6 (Hassan et al., 2004). Growth factors, for instance, basophils (CFU-Baso) megakaryocytes (CFU-Meg), erythrocytes (BFU-E) eosinophils (CFU-Eos) lymphocytes differentiate into progenitor cells in the bone marrow. Neutrophils and monocytes, on the other hand; rose from granulocyte-macrophage progenitor (CFU-GM) (Hassan et al., 2004). THE TYPES OF BONES MENTIONED IN THE QURAN AND HADITH.HEEL One of the bones mentioned in the Quran is the heel illustrated in Figure 7. Allah (The Most High) states: “My verses had already been recited to you, but you were turning back on your heels.!"[Quran, Surah Al Muminoon (The Believers), 23:66] The scholars mentioned concerning this verse that Allah (The Most High) called mankind but they refused and resisted in believing in Him (Ibn Kathir, 2000). From an anatomical perspective, the foot has three parts: forefoot, midfoot and hindfoot. The calcaneus (heel bone) is the largest tarsal bone in the hindfoot (AAOS, 2020). Figure 7: Anatomy of the back of the foot (Morton, 2016) CLAVICLE The clavicle (shoulder bone) is another type of bone mentioned in the Quran. Ibn Manzur (1993) mentioned about the following verse that the clavicle binds the neck to the shoulder region. “Yea, when (the soul) reaches to the collar-bone (in its exit).” [Quran, Surah Al Qiyamah (Judgement Day): 75:26]. Another reasoning narrated by Ibn Manzur (1993) is the presence of the two bones that associates the shoulder with the neck where the soul leaves the body between both clavicles during the death process. COCCYX The coccyx otherwise known as the tailbone; is a triangular bone that consists of 3 to 5 rudimentary coccygeal bounded segments in the terminal section of the vertebrae illustrated in Figure 8. The name is derived from the Greek phrase for a cuckoo bird's beak due to similar features (Lirette et al. 2014). The coccygeal cornu articulates the sacral cornua and is supported by the muscle: coccygeal gluteus maximus and; the ligaments - sacrotuberous and sacrospinous ligaments. The tendons on the lateral end are required for the bowel movement and supporting the pelvis during the seating posture that adds pressure to the coccyx (Lirette et al. 2014). Figure 8: The anatomical structure of the vertebrae. The coccyx has been mentioned in many hadiths that are summarised in Table 1. It can withstand pressure and cannot be destroyed by the decaying process of the corpse. It is described as ‘ajbu azzanab’ meaning 'the end of the final part of something'. The primitive streak that develops in the embryo in the 3rd-week shrinks and remains in the sacrococcygeal region and the stem cells adheres (Yusof et al., 2016). This may explain as to why teratoma, tumours of the coccygeal origin have a combination of different tissues: skin, bones, cartilage, muscles and teeth in comparison to tumours of other regions (Yusof et al. 2016). This further suggests as to why the coccyx is reconstructed during Judgement day. Despite the teeth is found in the coccyx - it is not a bone. They share similar commodities with the bone, for instance, the hydroxyapatite content. There is much evidence in the Quran and Hadith of cleansing the tooth and its benefits. This is particularly with the miswak which is from the branches of the arak tree. This has been consolidated by research conducted by Winarni et al. (2019) where miswak has antimicrobial properties and can improve the periodontal health. There are also spiritual benefits of the miswak where it was related from Aisha (may Allah have mercy upon her) that the Prophet (peace be upon him) said: “The merit of the salat performed after using a miswak is seventy times of the salat performed without using a miswak.” [Ahmad bin Hanbal, Musnad, VI, 272]. However, this hadith is not clear because the Hanafi school states that the merit occurs by using the miswak whilst performing ablution. On the other hand, the school of Shafi states that merit occurs when using the miswak before the prayer. Furthermore, Allah (The Most High) states in the following verse: “They say what! When we are reduced to bones and dust, should we really be raised (to be) a new creation?” [Quran, Surah Isra (The Night Journey) 17:49] Ibn Manzur (1993) mentioned about the verse that the bones remain after death, whereas the muscles and the varied types of the tissue will decompose into dust. Other scholars such as Ibn Kathir (2000) mentioned that 'dust' is concerning the soil. This illustrates the rigidity of the bone. Mujahid (may Allah have mercy upon him) thought that the verse was about those who disbelieve where the resurrection will not be a place of denial. Ali bin Abi Talha (may Allah have mercy upon him) reported from Ibn Abbas it regarding dust (Al Tabari 17:464). But Allah (The Most High) responds in another verse that after disintegration, one can be resurrected. "But now they ask mockingly, “Will we really be restored to our former state, even after we have been reduced to decayed bones?" [Quran, Surah An-Naziat (Those who drag forth), 79: 10-11] In another verse, The Almighty states: "And they argue with Us—forgetting they were created—saying, “Who will give life to decayed bones?” [Quran, Surah Ya-Sin, 36:78] Say, "Be you stones or iron", or whatever you think is harder to bring to life!” Then they will ask ˹you˺, “Who will bring us back ˹to life˺?” Say, “The One Who created you the first time.” They will then shake their heads at you and ask, “When will that be?” Say, “Perhaps it is soon!” [Quran, Surah Isra (The Night Journey) 17:50-51] The scholars, Mujahid, Said ibn Jubayr, Abu Salih, Al-Hasan, Qatadah and Ad-Dahhak agree that creating a substance is not difficult for Allah and if one was dead, Allah can easily resurrect (Al Tabari, 17:463; Ibn Kathir, 2000). Table 1: Evidence of the coccyx in the hadith OTHER FEATURES OF THE MUSCULOSKELETAL SYSTEM JOINTS A joint combines two or more bones to aid in mobility. The main types of joints are fibrous, synovial and cartilaginous and are dependent on the type of tissue and movement. For instance, a fibrous or cartilaginous are connected by connective tissue and does not have a bone cavity. The fibrous joint is found in the sutures of the skull, and the gomphosis of the teeth. Cartilage joints reside in the intervertebral joints and the symphysis pubis. On the other hand, a synovial joint is situated in the knee has a bone cavity. They have synovial fluid to remove friction which decreases contact between bones. Other examples are shoulder, hip and elbow. There are several sub-types of synovial joints: the hinge joint, ball and socket and the gliding saddle (Al-Najjar, 2005). Gliding joints are present in the wrists where flat bone surfaces glide freely in several directions. In total, there are 360 movable joints in the human body. 147 joints in the vertebral column, 24 joints in the thorax, 86 joints in the upper extremity, 92 joints in the lower extremity and 11 joints in the pelvis. The vertebral column has 25 joints between the vertebrae and 72 joints between the vertebrae and the ribs. The thorax has two joints between the sternal bones and thoracic cage, 18 joints between sternum and ribs, 2 joints between clavicle and scapulae and 2 joints between scapulae and thorax. The upper extremity has 2 joints between the scapular bone, 6 joints between elbows, 8 joints between the wrists and 70 joints between the hand bones. The lower extremity has 2 hip joints, 6 joints between knee bones, 6 joints between ankles and 74 joints between feet bones. The pelvis has 4 joints between coccyx vertebrae, 6 joints between the acetabulum bones and 1 joint of the pubic symphysis (Al Najjar, 2012). The hadith that confirms the total number of joints are as follows:Aisha (may Allah have mercy upon him) narrated that the Prophet (peace be upon him) said: "Everyone has been created with three hundred and sixty Joints. Whoever mentions Allah's greatness (says Allahu Akbar), praises Allah, extols Allah, and seeks forgiveness from Allah and removes stones from the path of the people, enjoins what is good and forbids the evil to the amount of those three hundred and sixty joints (sulama), he walks on that Day (of Judgment) having distanced himself from the Hell fire." Isn't this miraculous that the Prophet Muhammad (peace be upon him) precisely knew the number of movable joints ‘salama’ that many in the subsequent centuries could not identify an accurate number and have given estimates between 200 and 300 joints? The joints have also been associated with acts of goodness, for instance, giving charity, seeking His remembrance and forgiveness and acts of charity and evading evil. Abu Dharr (may Allah have mercy upon him) narrated that the Prophet (peace be upon him) said: "In every morning there is a charitable act on the joints of any of you. Every tasbihah (to say: subhanallah, i.e. Glory be to Allah) is a charitable act; every tahmidah (to say: al-hamdu lillah, i.e. Praise be to Allah) is a charitable act, every tahlilah (to say: la ilaha illallah, i.e. There is none worthy of worship but Allah) is a charitable act; every takbirah (to say: Allahu akbar, i.e. Allah is the Greatest) is a charitable act; enjoining the right is a charitable act; forbidding the evil is a charitable act. However, to fulfill that charity, it is sufficient to pray two rak'at of Duha." [Sahih Muslim] This emphasises how mankind should be grateful to Allah for the ability to move via our joints to do good charitable acts and even pray to Allah (The Most High). Scholars such as Ibn Hajar Al Asqalani encouraged mankind to do charity because of the body's natural phenomenon. Furthermore, there are several references to the joints in the Quran, Allah (The Most High) states: “(Remember) when your Lord revealed to the angels, verily, I am with you, so keep firm those who have believed. I will cast terror into the hearts of those who have disbelieved, so strike them over the necks, and smite over all their joints.'' [Quran, Surah Al Anfal, 8:12] Ibn Manzur (1993) mentioned that the joints or 'banaan' are the small joints in the fingers or can be from the lower and upper limbs but the verse is about all joints because they can be dissociated easily. MUSCLES The muscles aid in mechanical movement and how the musculotendon work is independent of the total joint work that is the time that joint power over a full gait cycle (Sasaki et al., 2009). It has been described in the Quran as 'flesh' in 23:14. Three types of muscles are characterised by their morphological features and type of movement. Skeletal muscle is a voluntary muscle that controls body movement. The smooth muscle conducts movement involuntarily via the autonomic nervous system and can be found in the hollow viscera walls of the gastrointestinal tract and respiratory tract. The cardiac muscle is found in the heart within the myocardium and in the aorta and vena cava vessels. It conducts an involuntary movement which is also controlled by the autonomic nervous system. Page (2012) described the skeletal and cardiac muscles with striated features. The skeletal muscles have bundles of myofibres that contains myofibrils and sarcomere. The myofibres produce fascicles that create the muscle tissue where the extracellular matrix and cytoskeletal proteins encompass each muscle layer. Its function is to maintain energy metabolism and cellular homeostasis (Mukund and Subramaniam, 2019). Skeletal muscle comprises of the autonomic nerves to facilitate the transmission of impulses and has a regulatory framework to maintain cellular homeostasis and oxygen levels (Mukund and Subramaniam, 2019). Dysregulation of the muscle contraction can be caused by environmental stress, for instance, oxidative stress and inflammation that can cause fibrosis, hypertrophy and atrophy (Mukund and Subramaniam, 2019). The movement of the synovial joints is dependent on the range of motion (ROM), that involves the muscles and joints. The muscle serves as a tension mechanism where passive muscle tension depends on the fascia and viscoelastic properties whereas active tension occurs in dynamic muscles and have neuroreflexive properties that involve alpha and gamma motor neurons (Page, 2012). The contraction of the skeletal and cardiac muscles is achieved by the depolarization of the calcium ion voltage-gated channels that open in response to the action potential. The neurotransmitter is released and; the depolarization spreads whereby dihydropyridine receptors in the skeletal muscles increase calcium ions that bind to Troponin C to form a cross bridge. Myosin bind to the actin when tropomyosin moved. Adenosine diphosphate (ADP) is released that causes the muscle to contract. The myosin head is released where the cycle repeats (Shreshta, 2015) Similarly, for the smooth muscle to contract, action potential causes calcium ion voltage-gated channels to open. However, the calcium binds to calmodulin as opposed to Troponin C. The enzyme myosin light chain kinase is activated and, the myosin causes muscle contraction. bone tumoursAlterations in the cellular features of the bone and dysregulation of the bone homeostasis can cause tumorigenesis. Tumour cells can metabolically aid osteoblasts and osteoclasts to increase aggressiveness (Sousa and Clezardin, 2018). It is vital to understand the normal histological structure and function of the bone and; how the pathophysiological mechanisms develop to research and manufacture novel therapeutic interventions (Fornetti et al. 2018). Sarcomas are tumours of the connective and support tissues that occur in bone, blood vessels, cartilage and fat tissues. Bone sarcomas arise from mesenchymal cells and stromal cells (Cortini et al. 2019). Stromal cells facilitate the tumour development and are formed by osteoblasts, osteoclasts, immunological factors and mesenchymal stem (MSC) cells (Cortini et al. 2019, Tzelepi et al. 2000). MSC cells derived from the adult bone marrow can differentiate with a doubling time of two days where under culture conditions it is ca. 6 fold. They are positive for several immunological markers: CD29, CD166, CD44 and CS105 (Hassan et al. 2004). Amongst the malignant bone sarcomas are: osteosarcoma, Ewing sarcoma and chondrosarcoma that account to 70% of malignancies causing high rates of mortality and morbidity presented in Figure 9 (Rajani and Gibbs, 2012). The patient survival rate of bone sarcomas has improved due to presence of combinational (adjuvant) chemotherapy after tumour resection in the 1970s and 1990s; but cases are still high (Fornetti et al. 2018; Simpson et al. 2018). There is a high risk of drug resistance following chemotherapy and; this can lead to the development of metastasis in the lungs that is characterised by poor prognosis. The development of the tumours in the bone will be incurable and undergo palliative care. A combinational approach between doxorubicin and methotrexate or cisplatin can be achieved where ca. 70% with no metastasis whereas with metastasis ca. 20% (Rajani and Gibbs, 2012). Osteosarcomas arise in the juxtaepiphyseal region and medullary cavities in the metaphysis of long bones where it rapidly grows in the arms and legs. The primary bone tumour primarily occurs in children aged 10 to 25 and is the third most common cancer amongst children and adolescents after lymphomas and brain cancers (Wang et al., 2018). It is characterised by the presence of the osteoid tissue and irregular and disorganised structure of the bone caused by malignant MSC cells (Simpson et al. 2018; Picci, 2007). Osteosarcoma can be subdivided based on clinical, histological and radiographic evidence: Intramedullary (low-grade) and surface (high-grade) (Misserschmit et al. 2009). Intramedullary osteosarcoma comprises of the destruction of the cancellous and cortical bone with the soft tissue extension. There are ca. 2% of osteoid tissue present in the diaphysis and metaphysis of long bones that can be misinterpreted to the benign lesion or fibrous dysplasia (Rajani and Gibbs, 2012). It is treated with neoadjuvant chemotherapy. Periosteal sarcoma are chondroblasts where some osteoid tissue are formed (Rajani and Gibbs, 2012) The pathophysiology of osteosarcoma is not well understood, however, the genetic factors have primarily contributed to tumorigenesis and tumour development. It can occur sporadically because of mutations in genes that encode for the proteins involved in the cell cycle regulation (Misaghi et al. 2018; Wang et al. 2018). For instance, Inactivation of the tumour suppressor genes; p53 and retinoblastoma (RB) and overexpression of MDM2 can cause bone tumour cells to proliferate. Mutations in the chromosomal number 17p13 can cause Li Fraumeni syndrome and the uncontrolled proliferation of cells are apparent (Simpson et al. 2018; Lietke et al. 2014). Additional alterations can occur in the BLM and RECQL4 genes that encode DNA helicases who function in unwinding the double-stranded DNA for replication – this leads to genetic syndromes such as Bloom and Rothmund-Thomson syndrome (Simpson et al. 2018). Staging of the tumour involves local and distant radiographical imaging of the destruction of the bone and the medullary bone soft tissue. Magnetic Resonance Imaging (MRI) presents the neurovascular structures and the metastasis, whereas the CT scan presents the pulmonary metastasis that occurs in the lungs. Response to chemotherapy can be determined by the Positron Emission Tomography (PET) (Rajani and Gibbs (2012). Other diagnostic radiological imaging used to evaluate the tumour are dynamic bone scintigraphy and angiography. To confirm the diagnosis of osteosarcoma, a biopsy is also requested (Picci, 2007). This presents progress in the diagnostic methods for osteosarcoma. Furthermore, amputation was commonly performed in the past, however; the survival rate was minimal in comparison to today where treatment is more advanced (Picci, 2007). Today, ITAP implants occur in patients with amputations. Besides, mTOR inhibitors (mammalian target of rapamycin) inhibitors were used for combinational therapy. mTOR is a phosphatidylinositol 3’ kinase (PI3K) serine-threonine that phosphorylates downstream signalling pathways to induce DNA repair and increase cellular proliferation. Also, the PI3K/AKT/MAPK pathway is also influenced by the insulin-like growth factor. Figure 9 - Examples of bone tumours EWING SARCOMA The following osteosarcoma is the most common paediatric malignancy and is characterised by round blue cells. Ewing sarcoma is caused by the chromosomal translocation (11;22)(q24;q12) that encode the EWS/FLI oncoprotein to maintain the malignant phenotype (Rajani and Gibbs, 2012; de Alava et al. 2013). To diagnose Ewing Sarcoma, it requires a range of molecular diagnostic methods to detect fusion genes of ETS family, histological and immunological techniques (Osaki, 2015; Delattre et al. 1992). Recent studies using the electron microscope and immunohistochemistry techniques suggests it has a neurogenic origin (Osaki, 2015). The standard treatment for Ewing Sarcoma is intense neoadjuvant and adjuvant chemotherapy (Osaki, 2015). This is normally doxorubicin, vincristine, etoposide, cyclophosphamide, ifosfamide and actinomycin-D (Osaki, 2015). There can also be a combined therapeutic approach which has proven effective: vincristine, doxorubicin and cyclophosphamide with radiation and surgery (Rajani and Gibbs, 2012). CHONDROSARCOMA Conventional chondrosarcomas account for most of the incidence of chondrosarcoma. They are mesenchymal tumours that affect the cartilage cells in the craniofacial and can also initiate in the intramedullary cavities of the femur, pelvis, shoulder, hip and, ribs (Rajani and Gibbs, 2012). Dedifferentiated chondrosarcomas occur in the chondroid areas of the pelvis and long bones and account for ca. 10% of chondrosarcomas (Boehme et al. 2018). Secondary chondrosarcomas, for instance, enchondromas, develop from cartilage lesions. Peripheral chondrosarcomas are caused by benign paediatric bone tumours called osteochondromas. Clear cell chondrosarcomas are rare low-grade tumours that occur in the epiphysis in the bone (Boehme et al., 2018). Chondrosarcoma is caused by the Hedgehog signalling and alterations in p53 and RB genes that affect the cell cycle regulation, migration, proliferation, angiogenesis and; other hallmarks of cancer (Rajani and Gibbs, 2012). Furthermore, chondrosarcoma cells are characterised by the loss of primary cilia which is caused by histone deacetylase 6 (HDAC6) which in turn induces tumour proliferation (Boehme et al., 2018). It is treated with chemotherapy. OTHER BONE TUMOURS Osteomas are benign tumours caused by the chromosomal alteration of 5 and can also cause Gardener's syndrome. Tumours arising in the skull, femur, tibia and vertebrae. Leiomyosarcoma occurs in the blood and organs. Leiomyomas reside in the fibroids and the lining of blood vessels in uterine cells. Rhabodomyomas soft tissue sarcoma develops in the voluntary muscles, nerves, fat, blood vessels, cartilage and bones in the head, neck and gastrointestinal tract of paediatric patients. Giant cell tumours have a soap bubble appearance and affect long bones and joints in the thighbone (femur) and shinbone (knee joint). This highlights there is a range of different types of bone tumours and recent studies have shown that 3D culture models are a novel approach in investigating tumour cells and its microenvironment to module the paracrine response, resistance to tumour drugs and the aggressiveness of tumours than rodent models (Cortini et al., 2019). Overall, the bone is an interesting source and the structure, function and physiology have been presented in the Quran, Hadith and literature work. Despite, the Quran is not a scientific book, it continues to serve as a fundamental purpose and guidance alongside the Mustalahul Hadith (authenticity of the hadith) where some of its verses provide scientific evidence that is progressively unrevealed by modern medical and scientific research. Next month, it will be the last section of my research project; where I will discuss the anatomy and physiology of the intestines and; the evidence found in the Quran and Hadith. The muscle in the intestinal wall aids in the digestion and absorption of food. Furthermore, Zhang et al. (2018) revealed that the intestinal microbial flora has a functioning role in bone health whereby it can dysregulate bone homeostasis by evading osteogenesis and inhibiting osteoblastic and osteoclastic activity by upregulating genes and growth factors that alter the hormones that play a role in the bone metabolism, for instance, cortisol, androgens and serotonin and this in turn; affects the bone mass. REFERENCESAAOS (2020) Calcaneus (Heel Bone) Fractures Available [online] https://orthoinfo.aaos.org/en/diseases--conditions/calcaneus-heel-bone-fractures/
Ahmad, Y. (2010) Islamic medicine: A key to better life. Saudi Arabia: Darussalam. Al‐Bari, A. and Al Mamun, A., (2020) Current advances in regulation of bone homeostasis. FASEB BioAdvances, 2(11), pp.668-679. Al-Hakim, S. (1968) al-Mustadrik alá al-Sahihayn fi al-hadith. wa-fi dhaylihi Talkhis al-Mustadrik. Egypt: Maktabat wa-Matabi al-Nasr al-Hadithah Allied Academies (2020) Bone Marrow Articles Open Access. Available [online] https://www.alliedacademies.org/scientific-journals/bone-marrow-articles-open-access-16112.html Al-Najjar, Z. (2005) Wonderful Scientific Signs in the Qur’aan UK: Al Hijaz Al-Tabari, A. (2001) Tafsir Al Tabari: Jami Al Bayan An Ta'Wil Aayi al Qur'an. USA: Darussalam. Boehme, K., Schleicher, S., Traub, F. and Rolauffs, B., (2018) Chondrosarcoma: A Rare Misfortune in Aging Human Cartilage? The Role of Stem and Progenitor Cells in Proliferation, Malignant Degeneration and Therapeutic Resistance. International Journal of Molecular Sciences, 19(1), p.311. Canalis, E., Economides, A. and Gazzerro, E., (2003) Bone Morphogenetic Proteins, Their Antagonists, and the Skeleton. Endocrine Reviews, 24(2), pp.218-235. Clarke, B., (2008) Normal Bone Anatomy and Physiology. Clinical Journal of the American Society of Nephrology, 3(Supplement 3), pp.S131-S139. Cortini, M., Baldini, N. and Avnet, S., (2019) New Advances in the Study of Bone Tumors: A Lesson From the 3D Environment. Frontiers in Physiology, 10.814. Creative Biomart (2020) ‘Skeletal development Proteins’ Available [online]:https://www.creativebiomart.net/researcharea-skeletal-development-proteins_819.htm Dallas, S., Prideaux, M. and Bonewald, L., (2013) The Osteocyte: An Endocrine Cell … and More. Endocrine Reviews, 34(5), pp.658-690. De Alava, E., Lessnick, S.L. and Sorensen, P.H., Ewing Sarcoma (2013) In: Fletcher, C.D.M., Bridge, J.A., Hogendoorn, P.C.W., Mertens, F., editors. WHO classification of tumours of soft tissue and bone. Lyon: WHO Press. pp. 305–309. Delattre, O., Zucman, J., Plougastel, B., Desmaze, C., Melot, T., Peter, M., Kovar, H., Joubert, I., de Jong, P., Rouleau, G., Aurias, A.and Thomas, G. (1992) Gene fusion with an ETS DNA-binding domain caused by chromosome translocation in human tumours. Nature. 359(6391):pp.162–165. Ducy, P., Zhang, R., Geoffroy, V., Ridall, A.L., and Karsenty, G. (1997) Osf2/Cbfa1: a transcriptional activator of osteoblast differentiation. Cell. 89(5) pp. 747-754. Eriksen, E.F., Axelrod, D.W. and Melsen, F. (1994) Bone Histomorphometry, New York: Raven Press, pp1 –12. Fawwaz, Z. (1999) Al-Durr Al-Manthur fi Tabaqat Rabbat Al-Khudur Beirut: Dar al-Kutub al-Ilmiyah; al-Tabah. Fornetti, J., Welm, A. and Stewart, S., (2018) Understanding the Bone in Cancer Metastasis. Journal of Bone and Mineral Research, 33(12), pp.2099-2113. Florencio-Silva, R., Sasso, G., Sasso-Cerri, E., Simões, M. and Cerri, P., (2015) Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. BioMed Research International, 2015, pp.1-17. Fukumoto, S., and Martin, T.J. (2009) Bone as an endocrine organ. Trends in Endocrinology and Metabolism 20 (5), pp. 230-236. Hassan, H. and El-Sheemy, M., (2004) Adult bone-marrow stem cells and their potential in medicine. JRSM, 97(10), pp.465-471. Ibn Hatim Tafsir Al-Quran Al-Azim Saudi Arabia: Maktaba Nizar Al-Baz. Ibn Kathir (2000) Tafsir Ibn Kathir. Saudi Arabia: Darussalam. Ibn Manzur, M. (1993) Lisan Al-Arab Beirut: Dar Ihyaa Al-Turath Al-Arabi. Imster, E. (2019) A few favorite snowflake photos Available [online] https://earthsky.org/earth/best-snowflakes-photos-from-earthsky-friends Karsten, E., Breen, E. and Herbert, B.R. (2018) Red blood cells are dynamic reservoirs of cytokines. Scientific Reports 8, 3101. Lirette, L. S., Chaiban, G., Tolba, R., & Eissa, H. (2014). Coccydynia: an overview of the anatomy, etiology, and treatment of coccyx pain. The Ochsner journal, 14(1), 84–87. Luetke, A., Meyers, P.A., Lewis, I. and Juergens, H., (2014) Osteosarcoma treatment – where do we stand? A state of the art review. Cancer Treatment Reviews. 40(4): pp. 523-532. Marks, S.C. and Popoff, S.N. (1988) Bone cell biology: the regulation of development, structure, and function in the skeleton. American Journal of Anatomy, 183 (1), pp. 1–44. Messerschmitt, P.J.; Garcia, R.M; Abdul-Karim, F.W; Greenfield, E.M and Getty, P.J. (2009) Osteosarcoma, Journal of the American Academy of Orthopaedic Surgeons: 17(8) – pp. 515-527 Misaghi, A., Goldin, A., Awad, M. and Kulidjian, A., (2018) Osteosarcoma: a comprehensive review. SICOT-J, 4, p.12. Moore, K. L. and Persaud, T. V. N. (1998) The developing human: clinically oriented embryology. 6th ed. Philadelphia: Elsevier Saunders. Morton, S., Newth, A. and Majeed, A., (2016) Pain at the back of the heel. BMJ, p.i1366. Mukund, K. and Subramaniam, S., (2019) Skeletal muscle: A review of molecular structure and function, in health and disease. Wiley Interdisciplinary Reviews: Systems Biology and Medicine. 12(1): e1462 Nollet, M., Santucci-Darmanin, S., Breuil, V., Al-Sahlanee, R., Cros, C., Topi, M., Momier, D., Samson, M., Pagnotta, S., Cailleteau, L., Battaglia, S., Farlay, D., Dacquin, R., Barois, N., Jurdic, P., Boivin, G., Heymann, D., Lafont, F., Lu, S., Dempster, D., Carle, G. and Pierrefite-Carle, V., (2014) Autophagy in osteoblasts is involved in mineralization and bone homeostasis. Autophagy, 10(11), pp.1965-1977. OpenStaxCollege, (n.d.) ‘Bone Structure’ Available [Online]: http://pressbooks-dev.oer.hawaii.edu/anatomyandphysiology/chapter/bone-structure/ Page P. (2012). Current concepts in muscle stretching for exercise and rehabilitation. International journal of sports physical therapy, 7(1), 109–119. Picci, P., (2007) Osteosarcoma (Osteogenic sarcoma). Orphanet Journal of Rare Diseases, 2(6). Qutb, S., and Salahi, A. (2015) In the Shade of the Qur'an (Fi Zilal al-Qur'an): Surah 33 Ahzab - Surah 39 Al-Zumar: v. 14 UK: The Islamic Foundation. Rajani, R. and Gibbs, C., (2012) Treatment of Bone Tumors. Surgical Pathology Clinics, 5(1), pp.301-318. Ralston, S., (2017) Bone structure and metabolism. Medicine, 45(9), pp.560-564. Sadler, T. W. (2010) Langman's medical embryology.11th ed. Philadelphia: Lippincott William & Wilkins. Sasaki, K., Neptune, R. and Kautz, S., (2009) The relationships between muscle, external, internal and joint mechanical work during normal walking. Journal of Experimental Biology, 212(5), pp.738-744. Schaffler, M.B., Cheung, W-Y., Majeska, R., and Kennedy, O. (2014) Osteocytes: master orchestrators of bone. Calcified Tissue International 94(1), pp. 5-24. Scheuer, L. and Black, S. (2000) Developmental juvenile osteology. London: Elsevier Science. Shapiro, I. M., Layfield, R., Lotz, M., Settembre, C. and Whitehouse, C. (2014) Boning up on autophagy: the role of autophagy in skeletal biology. Autophagy 10, 7–19. Shrestha, S. (2010) Mechanism of Skeletal Muscle Contraction Available [online] https://medchrome.com/basic-science/physiology/mechanism-of-skeletal-muscle-contraction/ Simpson, E. and Brown, H., (2018) Understanding osteosarcomas. Journal of the American Academy of Physician Assistants, 31(8), pp.15-19. Travlos, G., (2006) Normal Structure, Function, and Histology of the Bone Marrow. Toxicologic Pathology, 34(5), pp.548-565. Tzelepi V., Tsamandas A.C., Zolota V., Scopa C.D. (2009) Bone Anatomy, Physiology and Function. In: Kardamakis D., Vassiliou V., Chow E. (eds) Bone Metastases. Cancer Metastasis – Biology and Treatment. 12, pp 3-30 Wang, L., Gebhardt, M. and Rainusso, N. (2018) Osteosarcoma: epidemiology, pathogenesis, clinical presentation, diagnosis, and histology. Available [online] www.uptodate.com/contents/osteosarcoma-epidemiology-pathogenesis-clinical-presentation-diagnosis-and-histology Winarni, Y., Haslinda, R. and Aspalilah, A., (2019) Miswak: The underutilized device and future challenges. Journal of Dentistry and Oral Hygiene, 11(2), pp.6-11. Wyganowska-Świątkowska, M. and Przystańska, A., (2010) The Meckel’s cartilage in human embryonic and early fetal periods. Anatomical Science International, 86(2), pp.98-107. Yin, X., Zhou, C., Li, J., Liu, R., Shi, B., Yuan, Q. and Zou, S., (2019) Autophagy in bone homeostasis and the onset of osteoporosis. Bone Research, 7(1). Young, B., Lowe, J. S., Stevens, A and Heath, J. W. (2006) Wheather’s functional histology: a text and colour atlas. 5th ed. Philadelphia: Churchill Livingstone Elsevier. Yusof, N., Che, N., Che, A. and Hassan, A. (2016) The anatomy of the musculoskeletal system in the light of Al Quran and hadith. In: 2nd World Congress on Integration and Islamicisation: Focus on Medical and Healthcare Science (2WCII 2016), 21st-23rd October 2016, Kuantan, Pahang. Zhang, J., Lu, Y., Wang, Y., Ren, X. and Han, J., (2018) The impact of the intestinal microbiome on bone health. Intractable & Rare Diseases Research, 7(3), pp.148-155. Zheng, L., Wang, W., Ni, J., Mao, X., Song, D., Liu, T., Wei, J. and Zhou, H., (2017) Role of autophagy in tumor necrosis factor-α-induced apoptosis of osteoblast cells. Journal of Investigative Medicine, 65(6), pp.1014-1020. Zhu, L., Chen, J., Zhang, J., Guo, C., Fan, W., Wang, Y. and Yan, Z., (2017) Parathyroid Hormone (PTH) Induces Autophagy to Protect Osteocyte Cell Survival from Dexamethasone Damage. Medical Science Monitor, 23, pp.4034-4040.
0 Comments
Leave a Reply. |
Archives
February 2021
Categories
All
|
© COPYRIGHT 2024. ALL RIGHTS RESERVED.
Proudly powered by Weebly



 RSS Feed
RSS Feed